Prior to a multiple myeloma diagnosis, many patients will have a precursor condition that causes changes in their bone marrow, but doesn’t cause the traditional symptoms or organ damage associated with myeloma.
These precursor conditions, known as either monoclonal gammopathy of undetermined significance (MGUS) or smoldering multiple myeloma (SMM) are often discovered accidentally during routine bloodwork or urine testing for other conditions.
Both MGUS and SMM cause plasma cells in the bone marrow to grow more rapidly than normal, which can produce abnormal antibodies, called M proteins, and can eventually develop into myeloma.
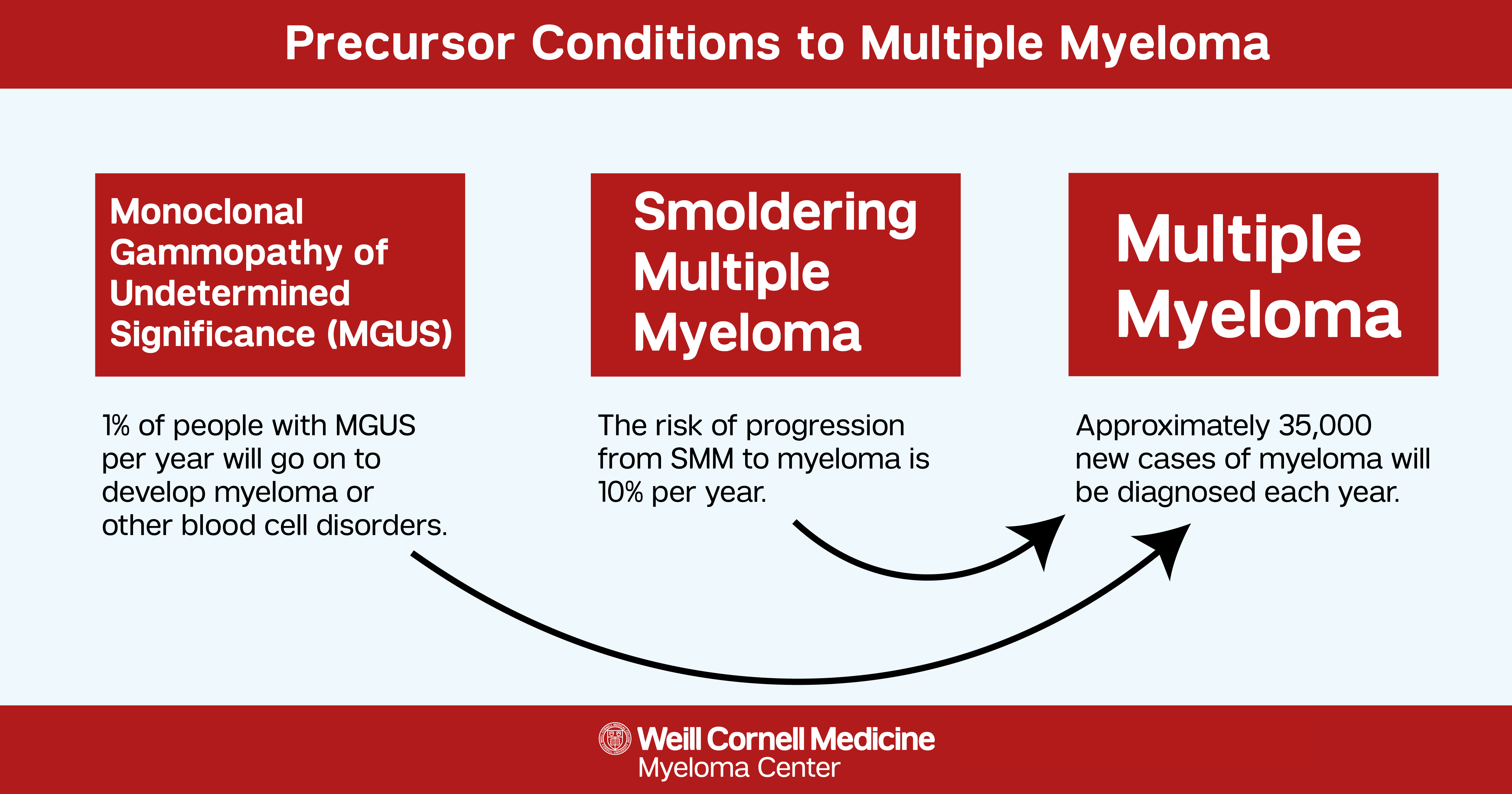
While unique diagnoses, these are considered part of the multiple myeloma disease spectrum. Typically MGUS presents as the first sign that something is awry. The risk of a patient's progression from MGUS to active myeloma is only 1% per year and approximately 20% of people with MGUS will progress to active myeloma in their lifetime. People who have smoldering myeloma have a higher risk of developing myeloma than those with MGUS and the risk of progressing to myeloma is 10% per year.
What makes MGUS different from Smoldering Myeloma?
Monoclonal gammopathy of undetermined significance (MGUS)
Monoclonal gammopathy of undetermined significance, or MGUS, is a blood disorder that occurs when bone marrow in the body produces abnormal plasma cells. Similar to multiple myeloma, these abnormal plasma cells create abnormal antibodies, called M proteins, that circulate in the blood stream. However, in MGUS, the abnormal cells only account for less than 10% of the cells in the bone marrow and typically don’t cause as many problems in the body.
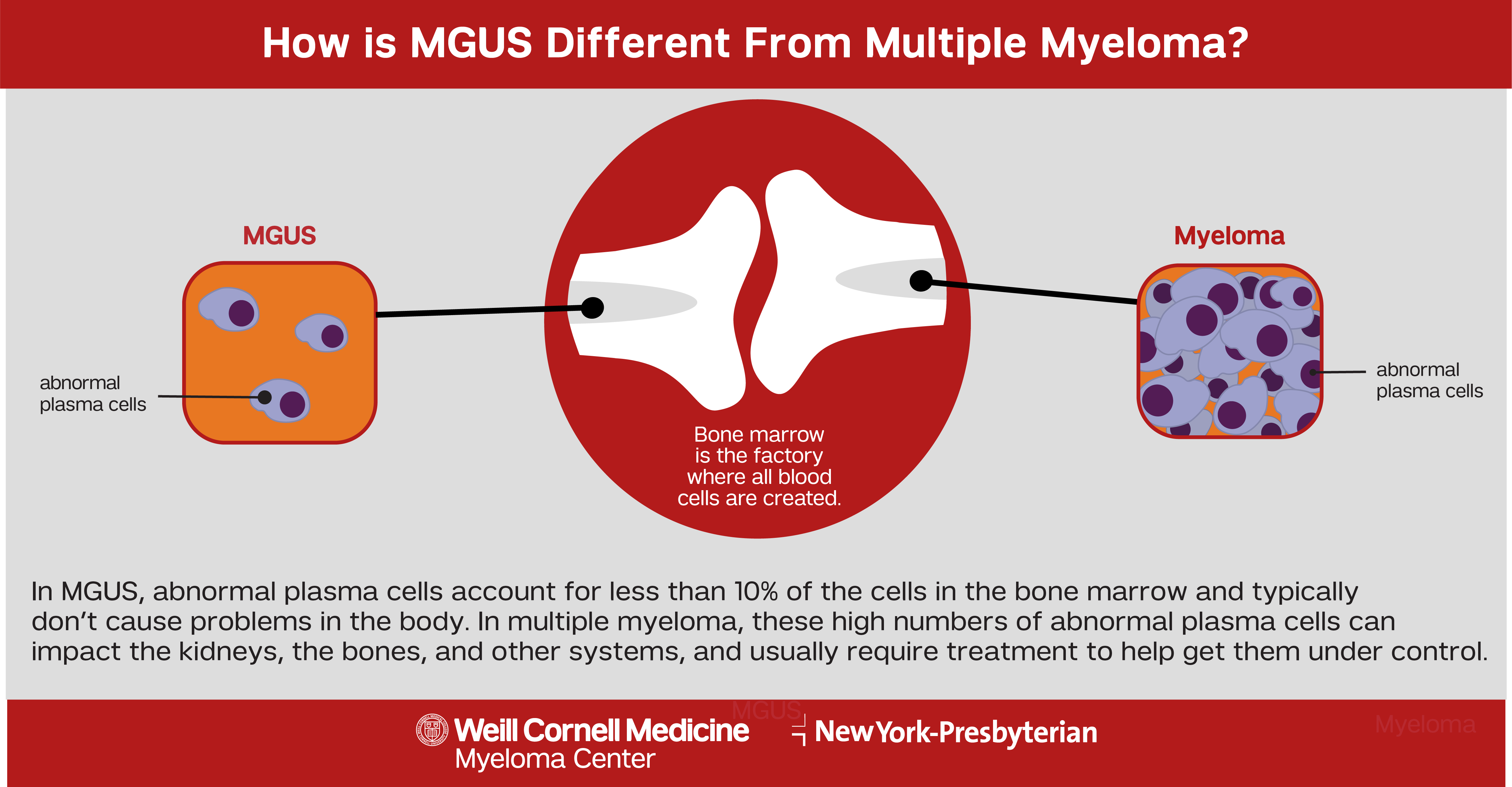
All blood cells are formed in the bone marrow by hematopoietic stem cells, creating the different types of blood cells in the body. Any interruptions to this process can create abnormal blood cells which can ultimately lead to the development of blood cancers.
MGUS is not classified as a cancer, but rather a pre-malignant condition, meaning an individual with MGUS may eventually develop a plasma cell disorder such as multiple myeloma or amyloidosis. In some cases, MGUS can turn into lymphoma if the damaged blood cells involve lymphocytes.
There is no standard treatment for MGUS, as interventions typically are not required. Instead, it’s important to continue regular checkups to monitor the M protein levels in the blood. Most people diagnosed with MGUS will not progress, but in the event that the disease does become multiple myeloma, regular checkups can allow people to catch the disease at an earlier stage and then start treatment.
Symptoms
MGUS often presents with no symptoms, but occasionally symptoms such as a rash or nerve problems like numbness or tingling may occur. Developing additional symptoms such as bone pain, fatigue, weakness, weight loss, fever, night sweats, headache, dizziness, nerve pain, bleeding, anemia, or swollen lymph nodes may indicate disease progression.
Although MGUS is usually silent and does not cause overt symptoms, rarely, monoclonal proteins can damage vital organs. This is usually suspected in individuals who present with unexplained symptoms. The kidneys, peripheral nerves, and skin can be among the organs most often affected. When this is suspected, a further work up might be warranted including biopsies or referral to a specialist such as a dermatologist, neurologist, or nephrologist. Treatment is available in certain cases including IV immunoglobulin, rituximab, and plasma cell–directed therapies.
Risk Factors
MGUS is typically seen in people over the age of 50 and risk increases with age. Although there is no known cause of MGUS, being male, of African descent, having a family history of plasma cell disorders, or having previous exposure to pesticides or insecticides can increase risk.
Smoldering multiple myeloma (SMM)
People with smoldering multiple myeloma (SMM) have higher levels of M proteins and abnormal plasma cells in the bone marrow than those with MGUS. SMM is considered an earlier version of multiple myeloma in which there are some overlapping signs and symptoms such as an increased amount of plasma cells in the bone marrow. However, in smoldering myeloma, these plasma cells have not yet accumulated or caused damage to the bones or organs.
This disorder affects everyone differently. For some people, it can take months to years for smoldering myeloma to become active myeloma. Some people with smoldering myeloma never develop active disease. However the risk of smoldering myeloma progression to active disease is greater than with MGUS.
If someone is diagnosed with SMM, it is very important to receive routine follow-up care to monitor for progression to multiple myeloma and if necessary, begin a treatment plan early. An initial smoldering multiple myeloma diagnosis does not usually require immediate treatment.
Symptoms
There are typically no symptoms associated with SMM. Most people are diagnosed during either routine blood tests or tests for other conditions. These blood tests may show the presence of abnormal antibodies, called M proteins, that indicate a plasma cell disorder, but this early stage does not usually have an impact on the body.
Risk Factors
It is unknown exactly what causes smoldering multiple myeloma, but older individuals, African Americans, and a males have an increased risk. Most people who develop SMM are over the age of 60.

